Last week, we hosted the fifth session of our webinar series on “Emerging Pathogens with a Special Focus on Flaviviruses.” This time, we had the pleasure of welcoming Dr. Miguel A. Martín-Acebes, senior scientist from INIA-CSIC, who shared insights into how the West Nile virus (WNV) manipulates the human body’s metabolism to survive and thrive. Dr. Martín-Acebes and his team have been investigating how WNV reprograms the host’s lipid and glucose metabolism, two essential systems that regulate energy and cellular structure. Their goal is to understand how the virus creates a more favorable environment for its replication and spread.
Using both infected mice and human samples from a 2020 outbreak in Spain, researchers discovered that WNV significantly alters lipid levels in the blood, especially increasing molecules like ceramides and sphingomyelins. These changes were traced back to the liver, which plays a central role in lipid production. One of the findings was the use of a compound called BPTIP, designed to block ceramide production. While it didn’t reduce the amount of virus in the body, it did lower levels of inflammatory molecules, suggesting a potential way to ease symptoms and reduce disease severity.
The virus doesn’t stop at lipids, it also boosts glucose metabolism in the brain, increasing energy production through a process called glycolysis. This helps the virus replicate more efficiently but also contributes to inflammation. To counter this, the team tested two drugs: 2DG and DCA. While 2DG had limited impact, DCA showed promise, reducing both the viral load and inflammation. This opens the door to new treatment strategies that don’t attack the virus directly but instead disrupt the environment it needs to survive.
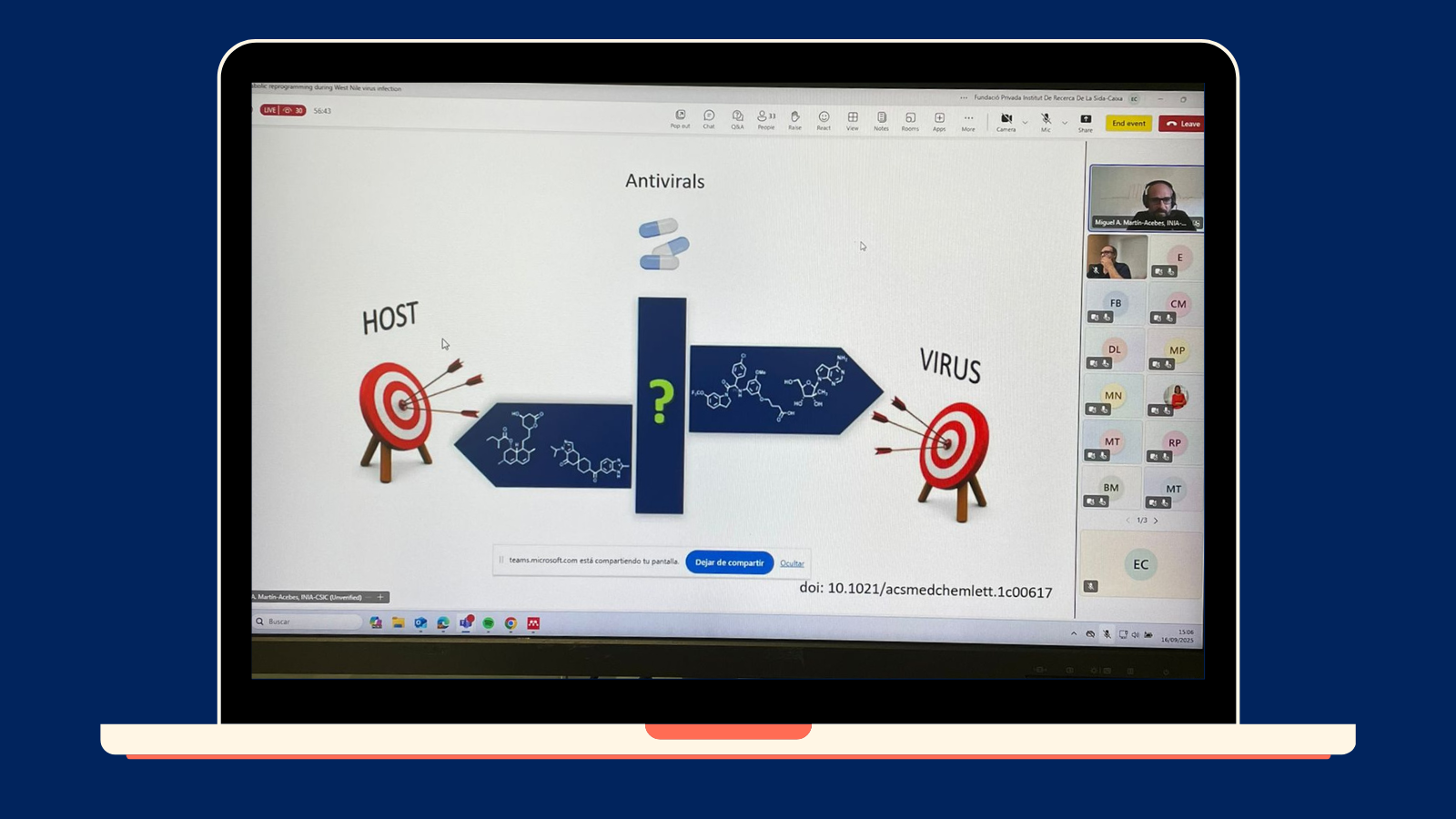
This research highlights a powerful new approach to antiviral therapy: targeting the host’s metabolic pathways rather than the virus itself. Such strategies could lead to broad-spectrum antivirals effective against multiple viruses, not just WNV. Dr. Martín-Acebes also emphasized the importance of understanding the immune system’s role in these metabolic changes. Inflammation itself can reshape metabolism, and future studies may explore how these findings apply to other diseases, including Alzheimer’s and multiple sclerosis.


